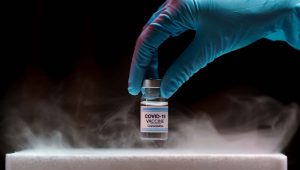
If the cold chain is not properly maintained, vaccine potency may be lost, resulting in a useless vaccine supply.
CDC Vaccine Storage and Handling Toolkit
Many vaccines contain living cells, and so when stored for any length of time they must be kept within a suitable temperature range to prevent degradation. Vaccine shots that are allowed to fall outside the safe storage range quickly lose their potency, meaning patients may be poorly immunized or even gain no protection at all.
This requirement to control vaccine temperatures at all times has led to the development of the cold chain: storage, transport and monitoring procedures that ensure potency is protected from the manufacturer all the way to each individual patient. But existing cold chain storage and monitoring measures may not cope with the extremely low temperatures required for some recently developed vaccines.
Vaccine Storage Temperatures
Many widely used vaccines require refrigerated storage between +2 and +8°C (+36 to +46°F), but are quickly damaged if allowed to freeze. These include vaccines for influenza, diphtheria and tetanus. Some other vaccines can tolerate being frozen, or even need sub-zero storage in the range -15 to -50°C (+5 to -58°F). This group includes vaccines for MMR and chickenpox.
But there is a trend emerging for vaccines that require storage at even lower temperatures. Since 2019 the first effective vaccines against Ebola have been approved for use, and these require storage at -60°C (-76°F). And some of the leading Covid-19 vaccine contenders, under development by Pfizer and Moderna, could need to be held as low as -80°C (-112°F).
These candidates are mRNA vaccines, a new gene-based technology at the cutting edge of vaccine development. Traditional vaccines are made up of small or inactivated doses of the whole disease-causing organism, or the proteins that it produces, which are introduced into the body to provoke the immune system into mounting a response.
In contrast, mRNA vaccines trick the body into producing some of the viral proteins itself. One important benefit is that the manufacturing process for mRNA vaccines is much faster, a vital consideration in the battle against Covid-19.
Maintaining the cold chain at these extremely low temperatures requires specialized packaging and handling procedures. It also presents challenges for monitoring the condition of vaccines.
I can’t emphasize enough the complexity of maintaining an absolute temperature from the depo to the distribution center to the airplane to the delivery truck to the surgery and the refrigerator in the doctors.
Nick Jackson, Head of Programs and Innovative Technologies at the Coalition for Epidemic Preparedness Innovations

Monitoring Vaccines at Deep Frozen Cryogenic Temperatures
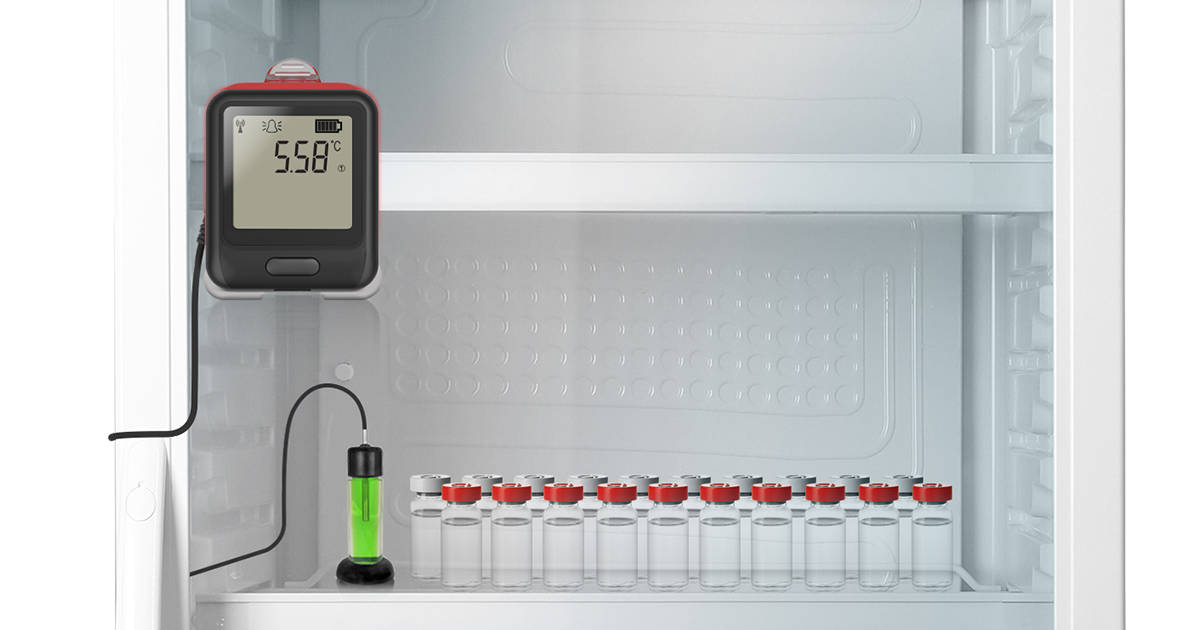
Every vaccine storage unit must have a Temperature Monitoring Device. An accurate temperature history that reflects actual vaccine temperatures is critical for protecting your vaccines.
CDC Vaccine Storage and Handling Toolkit
The approved method of monitoring vaccine storage temperatures is to use a Digital Data Logger. But many data loggers designed for monitoring existing refrigerated and frozen vaccine shots cannot measure accurately at deep frozen temperatures, or may not even work at all. The key limiting factor for low-temperature data loggers is the type of measurement sensor used.
Many vaccine loggers use a thermistor temperature probe, where the electrical resistance of the probe varies with temperature. Thermistors can offer high accuracy, typically ±0.1°C (±0.2°F), but do not work below -60°C (-76°F). For more extreme temperatures a thermocouple probe should be used instead.
Thermocouple probes contain two different conductive materials, and as the temperature changes a tiny electric current flows between them, the magnitude of the current varying with temperature. Although not quite as accurate as thermistors, thermocouples can measure all the way down -200°C (-328°F) and so are most suitable for cryogenic monitoring.
Conclusion
As health and medical services around the world make preparations for the first availability of a Covid-19 vaccine, the importance of low-temperature vaccine monitoring should not be overlooked. Relying on existing digital data loggers may not be sufficient, and organizations operating within the vaccine cold chain should ensure the availability of loggers suitable for monitoring deep frozen temperatures.
EasyLog offer a range of digital data loggers designed for monitoring vaccines in storage, including models suitable for cryogenic temperatures
References
Vaccine Storage and Handling Toolkit; Centers for Disease Control and Prevention, January 2020
Daunting task of distribution exposed as it emerges some vaccines must be ‘deep frozen’ at -70C by Sarah Newey and Jordan Kelly-Linden; Daily Telegraph, 8th September 2020
Covid-19 Vaccine Race Turns Deep Freezers Into a Hot Commodity by Jared S. Hopkins; Wall Street Journal, 4th September 2020
Five things you need to know about mRNA vaccines by Joanna Roberts; Horizon Magazine, 1st April 2020
Rapid Establishment of a Cold Chain Capacity of –60°C or Colder for the STRIVE Ebola Vaccine Trial During the Ebola Outbreak in Sierra Leone by Jusu, Glauser, Seward, Bawoh, Tempel, Friend, Littlefield, Lahai, Jalloh, Sesay, Caulker, Samai, Thomas, Farrell and Widdowson; The Journal of Infectious Diseases, Volume 217, Issue suppl_1, 15 June 2018, Pages S48–S55, 18th May 2018